Researchers from the Broad Institute of Harvard and MIT, the National Institutes of Health (NIH) and Vanderbilt University Medical Center for the first time have used a novel genome-editing technique to “rescue” mice from progeria, a rare genetic disease that causes accelerated aging.
Their findings, reported this week in the journal Nature, could lead to the first curative treatment for the disorder known as Hutchinson-Gilford progeria syndrome, which in humans causes premature aging and death from heart disease.
“While the idea of repairing mutant DNA is not new, this study is the first to demonstrate that a one-time systemic treatment with a base editor can precisely correct a DNA point mutation in multiple tissues and also improve lifespan,” said Jonathan Brown, MD, assistant professor of Medicine in the Division of Cardiovascular Medicine at VUMC.
Brown is the paper’s co-corresponding author with David Liu, PhD, who pioneered the “base-editing” technique at Harvard University, and NIH Director Francis Collins, MD, PhD, whose lab identified the genetic cause of progeria in 2003.
Base editing was inspired by the revolutionary genome editing technology known as CRISPR-Cas9, which can be used to correct defects in the sequence of nucleotides making up the base pairs, or building blocks, of the DNA “double helix.”
The molecular tool developed in Liu’s laboratory uses a novel variant of the Cas9 DNA-binding protein in combination with a guide RNA to zero in on the specific target gene sequence that is defective, and another enzyme to chemically convert the incorrect nucleotide back to the correct one.
The base editor is packaged within an adeno-associated virus (AAV), which does not cause disease in humans. When injected intravenously, the virus delivers its editing payload to tissues affected by the genetic mutation. Notably, this system does not require direct cutting of DNA and does not generate significant insertions or deletions, which are drawbacks of other CRISPR-Cas9 approaches.
“Five years ago we were still finishing the development of the very first base editor,” Liu said in a news release. “If you had told me then that within five years, a single dose of a base editor could address progeria in an animal at the DNA, RNA, protein, vascular pathology and lifespan levels, I would have said, ‘There’s no way.’
“It’s a real testament to the dedication of the team that made this work possible,” he said.
Progeria is caused by a cytosine-to-thymine base change in the nuclear lamin A gene. The mutation produces progerin, a toxic protein that affects multiple tissues and induces rapid aging, including bone and joint abnormalities, loss of muscle mass, skin changes and severe cardiovascular disease. Average life expectancy in children is about 14 years.
In the current study, the researchers tested the base-editing treatment in neonatal mice and also 14-day-old mice that carried two copies of the mutant lamin gene. A 14-day-old mouse is roughly equivalent to a human toddler.
Progeria mice that were given a single injection of the base editor at 14 days of life lived for about 17 months, over twice as long as untreated mice. On autopsy, treated mice showed no evidence in blood vessels of the cell death and fibrosis (scarring) that were extensive in the untreated mice.
“That was a really profound result,” Brown said, “because kids with progeria die of vascular disease. They suffer from heart attacks and strokes.”
”When my research lab identified the genetic cause of progeria in 2003, we hoped that someday this might lead to a way to help these children,” Collins said. “Along the way, we’ve made some progress with drug therapy, but the potential of actually correcting the fundamental cause at the DNA level is beyond anything we could have imagined back then.
“To see this dramatic response in our progeria mouse model is one of the most exciting therapeutic developments I have been part of in 40 years as a physician-scientist,” he said.
“It’s incredibly exciting to think that an idea you’ve been working on in the laboratory might actually have therapeutic benefit,” Brown added. “Ultimately our goal will be to try to develop this idea as a treatment for children with progeria, but there are key questions that we need to address first in these model systems.”
For one thing, some of the treated mice that lived a long time developed liver tumors. While there was no evidence the base editor was directly involved in tumor formation, AAV, which was used to deliver the base editor, is known to cause liver tumors in older mice.
“It is also theoretically possible the tumors arise in this mouse progeria model when the mice live longer, but we think if we can lower the dose of the virus, the potential for that problem diminishes,” Brown said. He also noted that liver tumors have not been observed in humans treated with AAV in clinical studies.
The researchers also are testing the effectiveness of the technique in older mice. “At what point in correcting a DNA mutation is it too late?” he asked. “If we treat more established disease, can we still achieve sufficient editing, and can that degree of editing still improve tissue function and block tissue damage?”
Brown said he became interested in progeria as a resident at Brigham and Women’s Hospital in Boston when he heard Collins give a lecture on the subject. “I was totally fascinated,” he said. “This was an example of how sequencing human genomes could reveal disease mechanisms and hopefully therapies.”
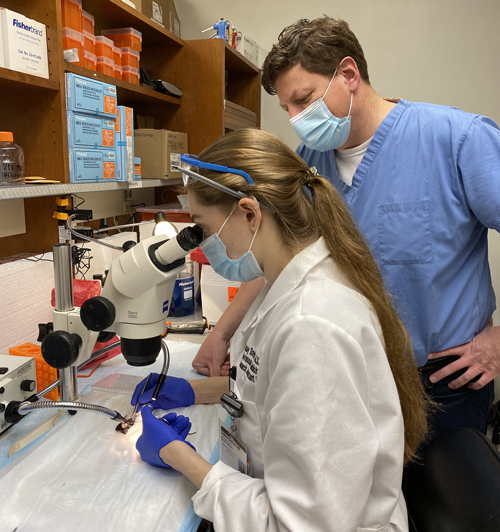
While finishing his postdoctoral work in Boston, Brown met Luke Koblan, who as a graduate student in the Liu lab contributed to the development of the base-editing technique and who is first author of the Nature paper published this week.
That’s how the three groups came together: Liu’s team had the editing tool, the Collins lab had developed a mouse model and had extensive expertise in progeria, and Brown and his colleagues performed initial experiments that suggested the technique might work. “It was very much a team effort,” he said.
Liu is Richard Merkin Professor and director of the Merkin Institute of Transformative Technologies in Healthcare at the Broad Institute, professor at Harvard University, and Howard Hughes Medical Institute investigator.
Also contributing to the paper were co-first author Michael Erdos, PhD, of the National Human Genome Research Institute, and Leslie Gordon, MD, PhD, co-founder of the Progeria Research Foundation, which coordinated the clinical trials that led to recent approval of the first treatment for this disease last month.
Other Vanderbilt coauthors were Lindsay Davison, Sean Doherty, and Quanhu Sheng, PhD.
To watch a video about the research, go here.
The research was supported in part by NIH grants AI142756, AI150551, TR002636, HG009490, EB022376, GM118062, HG200305, HL146654, HL126784, the Howard Hughes Medical Institute and the Progeria Research Foundation.












