Vanderbilt investigators and colleagues around the country have made a major discovery that could lead to better ways to treat type 1 diabetes (T1D).
The discovery concerns glucagon, a hormone that opposes the actions of insulin in regulating glucose levels in the bloodstream. These two hormones are secreted by different populations of cells in the islets of the pancreas: glucagon by alpha cells and insulin by beta cells.
T1D results from the autoimmune destruction of most insulin-producing beta cells in the pancreatic islet. Because of the lack of insulin, individuals must take daily insulin injections to control blood glucose. Yet a few beta cells persist in many people with T1D even 50 years after their initial diagnosis.
In a study of pancreas and islet tissue from individuals with T1D, the Vanderbilt investigators discovered that the remaining beta cells retained most features of normal beta cells and regulated insulin secretion. Further research is needed to determine whether these cells somehow escaped the auto-immune attack or were newly formed, and whether they can be protected and expanded.
Reporting March 6 in the journal Cell Reports, the researchers also showed that the alpha cells in these tissues did not secrete glucagon normally. They proposed that in alpha cells an abnormal amount of transcription factors, which regulate gene expression, leads to the impaired the secretion of glucagon.
Glucagon normally triggers the liver to produce more glucose when levels of this life-sustaining energy source — and the brain’s primary fuel — fall too low. Because individuals with T1D are known to have abnormal glucagon output, insulin treatment can unexpectedly lead to hypoglycemia (low blood glucose), which can cause confusion, seizures and loss of consciousness.
When islets from individuals with T1D were transplanted into a “normal” or non-diabetic environment, the abnormalities in alpha cells partially resolved. The researchers suggested that interventions might be developed to improve glucagon secretion and avoid the hypoglycemic complications of insulin treatment.
Much remains to be learned, but the Vanderbilt study has revealed important aspects of T1D and raises hopes that continued investment in basic research will eventually lead to an improved understanding of what causes T1D and ways to prevent or better treat it.
Until now, the mechanisms behind this impaired glucagon secretion in T1D were poorly understood. Vanderbilt’s paradigm-shifting discovery offers a new explanation for the impaired glucagon secretion in T1D and also suggests that targeting alpha cells may improve treatment of the disease.
Using research infrastructure and new approaches established by the Vanderbilt Diabetes Center, the researchers identified and collected tissue from individuals with T1D around the country who died of other causes and who had previously agreed to donate their pancreatic tissues for study. This is the first time that T1D islets, alpha cells and pancreatic tissue have been studied in such a detailed and comprehensive way from both physiologic and molecular standpoints.
The tissue was processed in collaboration with Rita Bottino, PhD, at the Allegheny Health Network Institute of Cellular Therapeutics in Pittsburgh, who pioneered methods for isolating pancreatic islets and tissue from the same T1D organ donor.
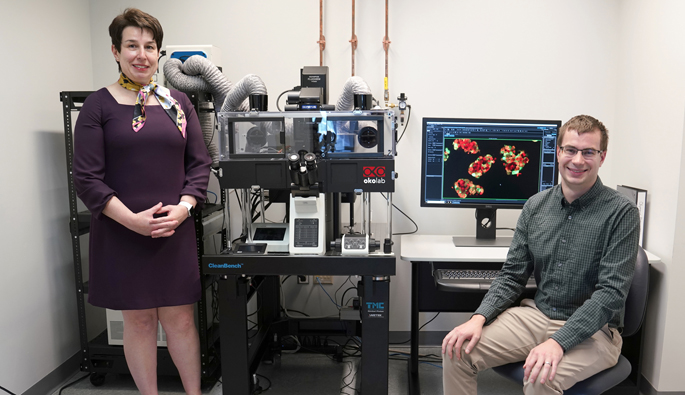
“It took us five years to collect the tissues and conduct these experiments,” said Marcela Brissova, PhD, research associate professor of Medicine in the Vanderbilt University School of Medicine.
Brissova was the study’s co-first author with MD/PhD student Rachana Haliyur, graduate student Diane Saunders and Shristi Shrestha, a graduate student at the University of Alabama Huntsville. She was co-corresponding author with Alvin Powers, MD, the Joe C. Davis Professor of Biomedical Science and director of the Vanderbilt Diabetes Center.
“This research reflects the broad and deep expertise in diabetes research and pancreatic islet biology at Vanderbilt,” Powers said. “This effort involved many investigators and institutions around the country with Vanderbilt as the hub.”
The research was supported by the Juvenile Diabetes Research Foundation (JDRF), the National Institutes of Health, the Human Islet Research Network (funded by the National Institute of Diabetes and Digestive and Kidney Diseases), the U.S. Department of Veterans Affairs and the Leona M. and Harry B. Helmsley Charitable Trust.
The research was conducted in collaboration with the JDRF-supported Network for Pancreatic Organ Donors with Diabetes, National Disease Research Interchange and International Institute for the Advancement of Medicine.
Other contributors included Vanderbilt faculty member Roland Stein, PhD, former faculty member Shawn Levy, PhD, now at HudsonAlpha Institute, and researchers from the University of Florida, University of Massachusetts, University of Chicago, La Jolla Institute for Allergy and Immunology and the Jackson Laboratory.