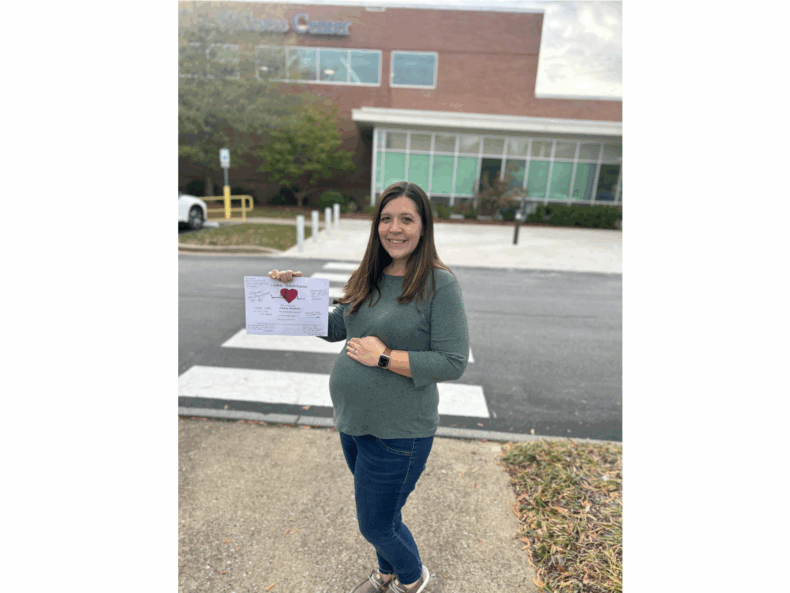
Esther Kim, MD, associate professor of Medicine at Vanderbilt, is part of a national effort to raise awareness about an uncommon cause of heart attacks in otherwise healthy, young and middle-aged women called spontaneous coronary artery dissection, or SCAD.
The rare condition is emerging as an important cause of acute coronary syndrome, myocardial infarction and sudden death. Kim and her colleagues want to spark change in the recognition, diagnosis and treatment of the poorly understood disease.
“Spontaneous Coronary Artery Dissection: Current State of the Science, A Scientific Statement from the American Heart Association,” was published recently in the journal Circulation.
SCAD occurs when a tear forms in one or more blood vessels, which can slow or block blood flow to the heart and trigger a heart attack. While it can affect older patients, and also men, SCAD is mostly found in middle–aged women, with the average age of presentation in the 50s.
“Because SCAD is becoming more widely recognized as an important cause of heart attack, there needs to be some guidance on how to diagnose, treat and manage this disease,” said Kim, co-chair of the scientific statement. “SCAD acts differently from heart attack caused by atherosclerotic coronary artery disease.
“It was necessary that we formulate a document to describe SCAD with an emphasis on the fact that the underlying physiology of this heart attack is not from cholesterol plaque and plaque rupture and thrombosis,” said Kim, who runs the Arteriopathy Clinic at Vanderbilt Heart and Vascular Institute (VHVI). “The tools we have now to treat heart attack — balloons, stents and blood thinning medications — were developed for heart attacks caused by cholesterol plaque. Using these same tools to treat heart attacks from SCAD may not result in the same success rates.”
SCAD occurs when the inner lining of the coronary artery splits and allows blood to seep into the adjacent layer, forming a blockage (hematoma) or continues to tear, creating a flap of tissue that blocks blood flow in the artery. It strikes without warning, traumatizing survivors. The cause of SCAD is currently unknown. Most doctors are unsure how to treat it.
“We need to raise awareness about SCAD,” Kim said. “This consensus statement is truly a call for more research and understanding of what causes it and how to prevent it.”
The statement culls information from experts who treat SCAD from across the country to develop a summary of the disease, including risk factors, diagnosis and treatment recommendations, potential triggers including stress or hormones, the prevalence of the disease among pregnant women and the connection it has with other arterial disorders including fibromuscular dysplasia (FMD) and aneurysmal disease.
“We continue to see both misdiagnosis and misunderstanding of SCAD,” said Kim. “A heightened suspicion of SCAD is required for an accurate diagnosis and appropriate treatment. This collaborative effort is essential in helping to spur change in our paradigm of care for SCAD patients,” she said.
The paper points to persistent gaps in knowledge about SCAD and the need for prospective and epidemiological studies in an effort to improve treatment and understanding of the disease.
Kim and her collaborators are hoping the statement will serve as a call to action among the medical community as well as a source of information among the patient population.