
Six years ago, Brenda Wilson, M.D., began experiencing foot pain that she describes as a pins and needles sensation.
Within a month, the pain was widespread and intense. Tightening and stiffening muscles, crippling fatigue and a lack of focus became disabling.
Desperate for answers, she sought help from myriad specialists. After years of wandering through the medical maze, she was diagnosed with fibromyalgia, a chronic pain condition that affects 4 percent of the U.S. population.
“Despite getting a diagnosis, I was unable to get relief from traditional treatments for fibromyalgia,” said Wilson, a psychiatrist. “I tried the different medications, physical therapies and chiropractic treatments available. My body just did not respond, and my condition continued to worsen.
“I just wanted my old life back,” she said. “It was becoming hard because I looked healthy on the outside so most people’s assumption was that nothing was wrong with me.”
At the recommendation of her internist, Wilson turned to the Osher Center for Integrative Medicine at Vanderbilt.
Formerly known as the Center for Integrative Health, the Center recently received a $5.5 million donation from San Francisco businessman Bernard Osher that will allow Vanderbilt to play an increasingly significant role in the integrative medicine domain while connecting it to the other four Osher Centers in the United States and Sweden. (See sidebar)
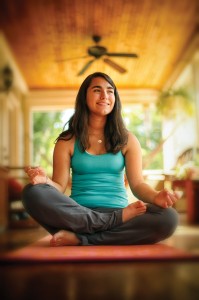
The Center opened in 2006, thanks to funding from John and Stephanie Ingram. It signaled a new era in medicine focused on developing clinical, educational and research programs providing relationship-centered care for the whole person, including mindfulness training, massage therapy, nutrition counseling, health coaching, acupuncture, physical therapy, yoga, tai chi, qigong, health psychology and integrative consultations by physicians and nurse practitioners.
The focus on healing has been reinforced through the generosity of Osher’s gift, who recognized Vanderbilt for its commitment to quality in the integrative medicine discipline. The Center has grown from a handful of referrals at the start of the program to more than 12,000 visits a year. In 2011 the Center nearly doubled its space and clinicians to meet the growing need and is now operating at full capacity in a nearly 9,000-square-foot facility at 3401 West End Ave.

“We are the only academic medical center in the Mid-South with an integrative medicine program,” said its medical director Roy Elam, M.D., associate professor of Medicine. “Most people come to us because they’ve tested the other possibilities for improving their health and have not found an answer. It is not infrequent for someone to come to us and say ‘I have been taking a handful of pills for five years and I am really tired of it. I want to make a change and I would prefer to use my own inner healing skills to care for myself.’
“Patients are looking for another way of living. Our very talented team of clinicians makes us special. Many of the patients we see today are overly extended and stressed. They are looking for alternative ways to manage their stress and health.”
Supporting the Whole Person
Wilson soon learned that managing her pain required a lifestyle change that was not going to be an easy fix.
“First and foremost they believed me,” Wilson said of the Center’s staff. “They believed that something was wrong even though I looked fine on the outside.
“The Center understood that not all conditions have lab work to verify what you are experiencing and to back up what you are saying. Because the staff here accepts you as a person and because of their approach to treating the whole person, they really embrace you,” said Wilson. “It was the first time I felt relief.”
Through the services offered at the Center, Wilson is learning how to live with chronic pain and taking steps toward building a new normal. She actively participates in tai chi and mindfulness training to help manage her pain.
Mindfulness training is a way of learning to relate skillfully to whatever is happening in your life, taking charge of your life, doing something for yourself that no one else can do for you—consciously and systematically working with your own stress, illness, and the challenges and demands of everyday life.
“The mindset is that you want this to be over with,” said Wilson. “But over time, I realized with their help that getting back to the life I knew might not be possible. I had to accept a new life. Every day I get up and accept that this is my life. I am always in pain, but I have learned to participate in life in a different way. I had to learn to take a breath.”
Learning to stop and breathe can change one’s approach to life’s challenges, said Tobi Fishel, Ph.D., director of Psychological Services at the Center.
“I think it is part of what we do here that is so helpful. We slow everything down. We teach people how to breathe slower and to notice and be more aware of their bodies. Our body signals are telling us things all the time, but we are not still enough to listen until often it’s too late.
“I find that incorporating the notion of just three breaths before every activity brings you right back to the present moment,” said Fishel. “Slow, deep breaths are calming. They decrease anxiety.”
A Stressed Out Nation
According to the American Psychological Association’s Stress in America™ survey, more adults report that their stress is increasing rather than decreasing, with 39 percent saying their stress had increased over the past year and even more saying that their stress had increased over the past five years (44 percent). Only 27 percent of adults reported that their stress has decreased in the past five years and fewer than a quarter of adults said that their stress has decreased in the past year (17 percent).
Over time, continued strain on your body from routine stress may lead to serious health problems, such as heart disease, high blood pressure, diabetes, depression, anxiety disorder and other illnesses, according to the National Institute of Mental Health.
“The level of stress related to chronic health conditions is out of control. We have to change what we are doing. We have to learn to slow down,” said Fishel, adding that integrative medicine is not designed to take the place of traditional models of care, rather it is used alongside conventional medicine.
Graciela Rayome, 16, who is being treated for type I diabetes, has worked with Fishel for five years to cope with her diagnosis and to work on communicating with her mom, Agnes, about her disease. She has also participated in several classes at the Center for teens with chronic illnesses.
Both mother and daughter admit to being overwhelmed with the management of Graciela’s disease, which includes wearing an insulin pump and a continuous glucose monitoring system as well as daily multiple blood glucose checks, calculations of dietetic intake and exercise documentation.
“Her diabetes management was quite involved and a bit complicated,” said Agnes. “What makes it hard is the mental and emotional part of it all.
“I know that I am overprotective of her, so the diabetes just added a whole other dimension to it. For me it’s the fear of what could happen if she is not with me and nobody knows how to help her. I am learning to trust Gracie’s ability to take care of herself.”
Agnes said Fishel has helped them both cope with the day-to-day diabetes requirements through yoga and mindfulness classes.
Graciela admits that she too can become anxious about spreading her wings, especially as she is nearing the driving age.
“Driving has been a recurring theme,” said Graciela. “We talk a lot about driving since my blood sugars fluctuate so much. Talking to Tobi has also been helpful when communicating with my mom about when I want to go to a sleepover, field trip or anything that would result from being away from her for long periods of time.
“The yoga and mindfulness classes have made a difference in my own anxiety and helped me feel more confident and sure of myself that I can do this,” she said.
Fishel said stress can further exacerbate a physical condition and the team at the Center works to ensure that every aspect of the patient’s life is considered when devising treatment plans.
Moving Beyond the Medicine Chest
Looking toward the future, Fishel and Elam hope that integrative medicine as a discipline is not functioning as a silo; rather the treatment modalities utilized at integrative medicine centers will become part of the medical treatment plan as a whole.

Bernard Osher’s gift will capitalize on the Center’s current success and move it forward to the next level. Today, the Center is perfectly positioned through its past work, this gift and the network of other centers, to achieve its goal of achieving interdisciplinary collaboration, which is the foundation of patient care throughout Vanderbilt.
“The team at the Center has helped us to introduce important concepts regarding complementary therapies throughout Vanderbilt’s required curriculum,” said Kim Lomis, M.D., associate dean for Undergraduate Medical Education at Vanderbilt University School of Medicine (VUSM).
“Students interested in more in-depth training also have the opportunity to participate in electives at the Center.”
VUSM offers a course called The Healers Art for first- and second-year medical students. The curriculum, led by Elam, allows students to interact in a compassionate, learning environment to identify personal and universal meaning in their daily experience of medicine. About 25 students are enrolled each year in the course.
Wilson, who has since given up her medical practice, applauds the process of teaching integrative health early in medical training.
“I feel that it must be introduced into the medical schools as a form of treatment that can enhance traditional medicine,” she said. “It is a marriage of medicines. And it must also be taught in continuing education settings for physicians. There needs to be an acceptance of this type of treatment along with traditional medicine.
“Integrative medicine is a tool much like medications—healing on different levels.”















