by Jill Clendening
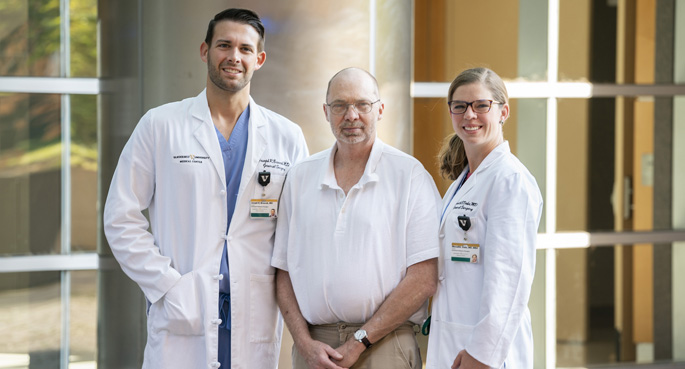
Nashville resident Keith Sanford runs out of fingers when he counts his past surgeries, including a kidney and pancreas transplant, so when his Vanderbilt Health surgeon gave him the option of having an abdominal hernia repaired with a minimally invasive, robot-assisted procedure, he agreed.
“She told me it was a way to avoid having another large incision,” he said. “After I had the surgery, there was a lot less pain and discomfort. I didn’t even think about taking any kind of pain medication afterward. There are five little incisions, and they’ve healed up fantastically. And the awful pain I was having with the hernia is gone, too.”
Vanderbilt University Medical Center is the only medical provider in Tennessee offering a robot-assisted, enhanced-view, totally extraperitoneal (eTEP) hernia repair, a minimally invasive procedure that replicates a traditional abdominal hernia repair that is performed with a large, open incision.
A hernia happens when an organ, intestine or fatty tissue squeezes through a gap or weak spot in muscle or connective tissue, and they occur most often in the abdomen. Hernia repair is one of the most common surgical procedures, with more than 1 million hernia repairs performed each year in the United States.
“We’re not changing how hernia repair is done; the addition of the robot allows us to do the same surgery, just through smaller incisions,” said Meredith Duke, MD, assistant professor of Surgery, one of three Vanderbilt Health surgeons who currently perform the procedure. “The robot also provides 10 times the magnification and three-dimensional visualization so we can see the arteries, nerves — all the things that we’re trying to protect — very well.”
The smaller incisions allow the insertion of robotic surgical tools, meaning there isn’t a large incision that can lead to a greater chance of post-operative complications such as surgical site infection and delayed healing. Reinforcing surgical mesh, even large, full-abdomen sheets, can also be placed through the small openings.
Other benefits of robot-assisted hernia repair are that there is often significantly less use of post-operative narcotics for pain management and the length of time in the hospital after surgery is often two or three days shorter than for an open abdominal hernia repair.
“When Dr. Duke came in the day after the surgery and said, ‘You’re ready to go home,’ I was honestly hesitant,” Sanford laughed. “With my personality, I was afraid I might try to jump right back into work.”
Nurses who see patients at post-surgery follow-up appointments who’ve had minimally invasive hernia repairs have also noticed changes.
“Patients are pleasantly surprised that they have recovered so well,” said Lisa Truett, MSN. “If they have had an open repair in the past, they usually mention things such as ‘less pain medications’ or ‘able to walk around easier than before.’ I’ve had several patients who have not taken any narcotics following minimally invasive surgery, and the majority are completely off of them when we see them back in clinic.”
At VUMC, each individual with a hernia is evaluated to determine if their specific case is suitable for a robot-assisted procedure, said Joseph Broucek, MD, assistant professor of Surgery. Vanderbilt Health surgeons perform around 10 robot-assisted hernia repairs each month.
Ideal surgical candidates have a lower body mass index (BMI) and have not used nicotine products within one month of surgery. Use of medications that can hinder healing, such as immunosuppressant drugs and steroids, is also evaluated, as well as health issues that can negatively impact recovery and healing, such as diabetes and heart disease.
If a medical team believes a surgical candidate can improve their post-operative recovery by addressing issues such as losing weight, quitting smoking or better disease management, they can be referred to other Vanderbilt Health providers to address those concerns before surgery is scheduled, said Broucek.
“Another advantage of offering this technique at Vanderbilt is that there’s great collaboration between surgeons, so we always have a second pair of hands available to assist if needed,” Broucek said. “We also have a large Hernia Center with a weekly, multidisciplinary hernia conference where we discuss our cases.”
Significant scar tissue, difficulty in removing mesh inserted during a prior surgery or internal tissue adhesions can sometimes lead to the need to covert from a minimally invasive procedure to an open surgery while in the operating room, and patients are advised of that possibility, said Duke.
In addition to Duke and Broucek, Richard Pierce, MD, assistant professor of Surgery, also performs the minimally-invasive, robot-assisted hernia repairs. All Vanderbilt Health surgeons who perform robot-assisted surgeries have received specialized training, such as a fellowship, in order to use the robots during procedures.
A surgical consultation for a minimally invasive robot assisted hernia repair can be scheduled by calling the Vanderbilt Hernia Center at 615-936-4500.