by Holly Fletcher

Income, education, access to healthy food and other factors influence a person’s health, so a newly established Office of Health Equity is designed to strengthen Vanderbilt University Medical Center’s programs and ties into networks around the region to improve the underlying elements.
Consuelo Wilkins, MD, MSCI, has been named to the newly created positions of Vice President for Health Equity at VUMC and Associate Dean for Health Equity with the Vanderbilt University School of Medicine.
Wilkins wants the realities of a person’s life and systematic barriers that prevent optimal health to be factored into the care they receive and find ways for community organizations to work with the Medical Center to help relieve burdens that can impede health. Wilkins plans to find ways to do broader scale research that considers biological, environmental and sociocultural factors that impact health.
“It’s about making sure we understand how income and access to food, for example, impact health and care and think about how to meet needs broadly,” said Wilkins. “If we’re not doing it in a way where we can actually speak to the social determinants or learn from them, then we are going to be missing important undercurrents.”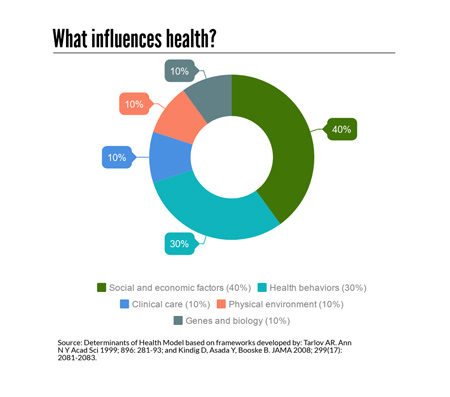
Here’s how Wilkins wants to think about health equity and what her initial priorities will be.
What’s the easiest way to define health equity?
Health equity is everyone having a fair opportunity to be healthy or as healthy as possible.
I think that health systems, organizations and communities, to the best of their ability, must try to remove the barriers to achieving health — and many of those are outside health care. It may be financial strain, food insecurity or limited health literacy.
It’s about making sure we are considering the needs broadly and not disadvantaging people who are already disadvantaged.
What’s a common misconception?
Some places include health equity with diversity and inclusion initiatives. A distinction I like to make is diversity and inclusion usually refers to the people who are providing the care (health care workforce) and those who are being educated and trained to do so.
Health equity is about outcomes. It means we are focusing on whether people have access to fair and just opportunities to access the care, understand the finances, implement the health management strategies. It’s easy to confuse the terms.
When some people think about health equity they are only thinking about racial and ethnic minorities — and certainly the history in this country make the health inequities more pronounced — but people are socially disadvantaged for many reasons, income and education, among them.
How would you characterize health equity as an idea in health care broadly — is it on the cusp of being widespread, is it fringe, or is established?
It depends on where you are. It’s still fringe and marginal, but I think there are several factors that are bringing it to the forefront. More organizations like the American Hospital Association are embedding health equity into strategic plans and I think more people and more organizations are recognizing that health equity isn’t about a few people; it’s about all of us.
What are some of your priorities?
There are dozens of initiatives and programs that are already happening here at VUMC, and the university and in Nashville. A recent effort to catalog them counted about 100, most of them are not connected, or if they are, it’s in varying degrees.
It will be important for us to understand what resources we have and what fantastic work is already occurring and how we can support it so we can find the gaps. We’ll take some time to understand the needs and priorities before we move forward.
We need a better connection internally. We also need a better connection to organizations and community partners — the people who are going to help address food insecurity, financial strain, job opportunities.
We also have to find a way to systematically collect social determinants as we provide health care. There are several factors to consider: how do we collect the information efficiently and accurately, how are we going to fit into the already busy clinical settings, how will we use this information to improve health.
And I want to help the institution think about the equity and health outcomes for the staff at VUMC. The financial strain and income levels are very different among employees — we are a microcosm of the city. The people in nutrition services and patient transport are very important parts of the health care system, but at the end of the day many of them are going back to neighborhoods with fewer resources. They live in food deserts or food swamps.












