Zoe Forman, 17, had one final number, a jazz routine, to perform in a Nashville dance competition in March. On the way to her wardrobe change, the Hoover, Alabama, native couldn’t catch her breath. “I can’t breathe; I can’t breathe,” her mom, Heather Rossomme, recalls Zoe saying.
Bystanders assumed the healthy teen — who has danced for nine years, six of those competitively — was overheated or exhausted. Conscious, though unresponsive to questions, Zoe quickly worsened. Another dancer’s grandfather, who is a doctor, stayed with her until an ambulance arrived to take her to Monroe Carell Jr. Children’s Hospital at Vanderbilt.
En route to the hospital, Zoe went into cardiac arrest. Her heart stopped. Rossomme sat in the front of the ambulance and typed one word via text to her husband: “Pray.”
Teamwork in action
At Monroe Carell, the emergency team performed CPR for what Rossomme estimated to be at least five minutes. “I did not look. I stood outside the door praying,” she said. “Finally, they got her heartbeat and then took her up to the floor and put her on ECMO (lung and heart support machine).” It was about four hours later at 3 a.m. that she saw her daughter.
Reflecting on that fateful day, Rossomme, a person of strong faith, believes her daughter was in exactly the right place when the heart issues started — a confluence of incredible people from the dance competition to the hospital. The next morning, Zoe was diagnosed via chest CT scan with anomalous aortic origin of a coronary artery (AAOCA), a rare congenital heart condition, which is also known to be the second leading cause of sudden cardiac death in young athletes.
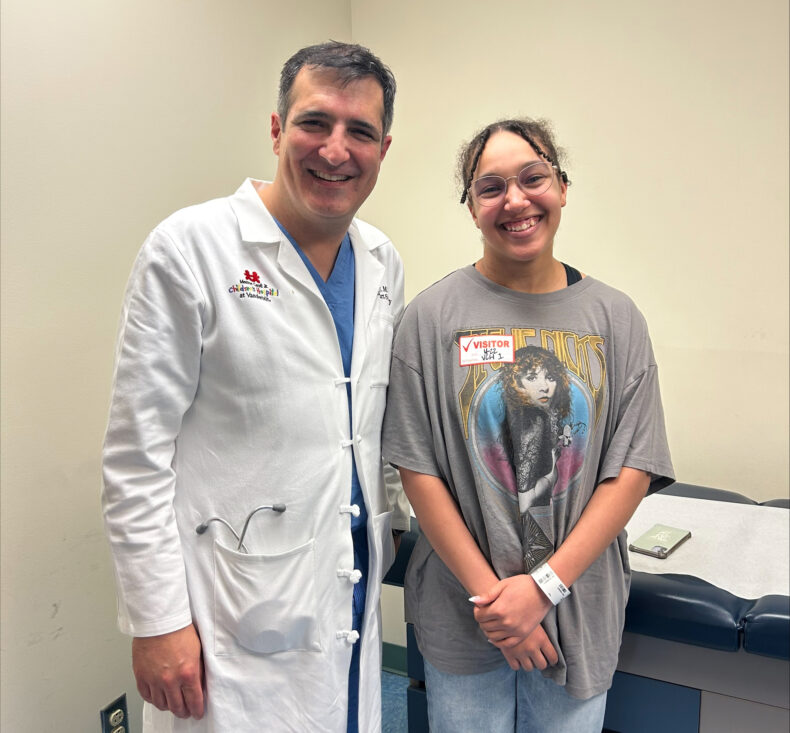
Monroe Carell is home to one of the leading experts in AAOCA, Carlos Mery, MD, MPH, chief of the Division of Pediatric Cardiac Surgery, who arrived at Vanderbilt just six months earlier and who is creating a dedicated pediatric cardiac anomalies clinic like he developed at his previous children’s hospital. Mery said AAOCA is often the cause of death for athletes who collapse during a sport but get help too late.
“She’s lucky to be alive. It’s a testament to a lot of people — at the dance competition, in the ED, the pediatric cardiac intensive care unit, the cardiology team,” Mery said. “Her care is also a testament to what multidisciplinary teams can do when we work together. Vanderbilt has created a structure that brings together the expertise to tackle difficult cases.”
He diagnosed Zoe with a form of AAOCA — anomalous left coronary artery with intramural segment, meaning the left coronary artery of her heart developed in the improper place, within the aortic wall.
With the left artery running through the aortic wall, it was being compressed and squeezed every time she exercised, restricting her blood flow. Essentially, she was a ticking time bomb.
When Mery first encountered Zoe on ECMO, her pulse was weak, and an echocardiogram showed the heart function was dismal — barely any movement of her heart muscles could be detected, he recalls.
“We were not sure the heart was going to recover,” Mery said. “We knew that if we were going to give her any chance, we had to act as soon as possible because that was the only way to salvage her heart.”
Rossomme said Mery told them that the left side of Zoe’s heart was only functioning at 8% and the team needed to operate.
“I asked him how confident he was in the procedure,” she said. “He very sweetly and humbly said, ‘This is my specialty,’ and then he explained his background. There was nothing to say but ‘yes.’ We went down to the chapel, waited and prayed.”
Complex surgery
The cardiac surgical team members began the six-hour surgery. They started by switching Zoe from the ECMO machine to a bypass machine, and they prepared to stop her heart using a potassium solution. While the heart was stopped, they performed an unroofing operation in which Mery excised the intramural segment from the aortic wall and relocated it to the correct side and position.
Then they had to restart Zoe’s heart — and wait. Would it regain function, and how much? As her heart restarted, they carefully and slowly weaned Zoe off the bypass machine.
“To our surprise, the function was almost normal at the end of the operation, and her echo looked great,” Mery said. “By the next morning, she was extubated, which is just amazing. It shows the plasticity of the heart and the ability for a young heart to recover after such a big event. And it also tells you how important it is to act on these quickly.”

Zoe was moved to the stepdown unit less than 48 hours postoperation. As she recovered, a brain scan showed she had suffered a mild stroke, likely when she was in cardiac arrest. Within a week, however, doctors saw no signs of brain injury, and with her heart functioning well, she was discharged from the hospital about seven days after the incident.
Zoe is back home in Alabama continuing to grow strong, and she is back to doing things she loves like crocheting. She will have a stress test in June to determine if she can return to dance.
“We were so blown away by everyone we came in contact with — every nurse, every doctor,” Rossomme said. “We had a very large awareness that we were exactly where we were supposed to be. Now, our mission is to spread the word and raise awareness.”
Expanding knowledge of the condition
Mery said there is still a lot to learn about AAOCA, such as who’s at risk for a cardiac event, how best to treat, if at all, and when? He has dedicated much of his career to researching the condition and helping put together care protocols for people who are diagnosed with it.
“There is still a lot that we don’t know about this disease,” he said. “For example, Zoe has exercised many times in her life, and probably even more than this time, but for some reason, something happened on that Saturday that was too much for her heart. And why then?”
At Monroe Carell, he is bringing together a dedicated team of cardiologists, radiologists, interventional cardiologists, electrophysiologists, surgeons and others for a comprehensive cardiac anomalies program.
“We’re looking at how do we move the needle to ensure that we have the best in care for these patients, and what makes us unique is that because we are a part of Vanderbilt University Medical Center, we can bring pediatric and adult cardiologists together to care for these patients over their lifespan.”


















