 The surgical team included, from left, Michael Topf, MD, Kyrionna Golliday, Carleigh Burns, Marcus Balanky, Jo Chung, and Eben Rosenthal, MD.
The surgical team included, from left, Michael Topf, MD, Kyrionna Golliday, Carleigh Burns, Marcus Balanky, Jo Chung, and Eben Rosenthal, MD.
Surgeons in Vanderbilt University Medical Center’s Department of Otolaryngology-Head and Neck Surgery have successfully performed the country’s first procedure using the latest generation of intraoperative PET (positron emission tomography) and CT (computed tomography) technology, with the goal of improving surgical outcomes.
Michael Topf, MD, associate professor of Otolaryngology-Head and Neck Surgery, performed the initial surgery along with several others in the weeks following as part of a study that seeks to demonstrate the long-term viability of the procedure, which uses a device developed by Belgium-based surgical technology company Xeos. As part of the study, up to 50 patients may undergo surgery with the support of the Aura 10 scanner.
During each surgery, the scanner is brought into the operating room to image a resected tumor. PET-CT combines the functional information gained through PET with the structural details gained by a CT scan, aiding in accurate staging, therapy response assessment and early detection of recurrent disease. The scanner provides surgeons an immediate, real-time view of the specimen, allowing them to immediately assess the success of the resection in achieving a negative margin.
A margin refers to the areas around the tumor being removed. The desirable outcome is to complete surgery with a negative margin, indicating that no cancer is found at the edge of the removed tissue. A positive margin indicates that cancer cells remain in the body, which increases the risk of recurrence and reduces the chance of survival. At VUMC, surgical teams take several approaches to achieving negative margins, including the use of fluorescence imaging agents.
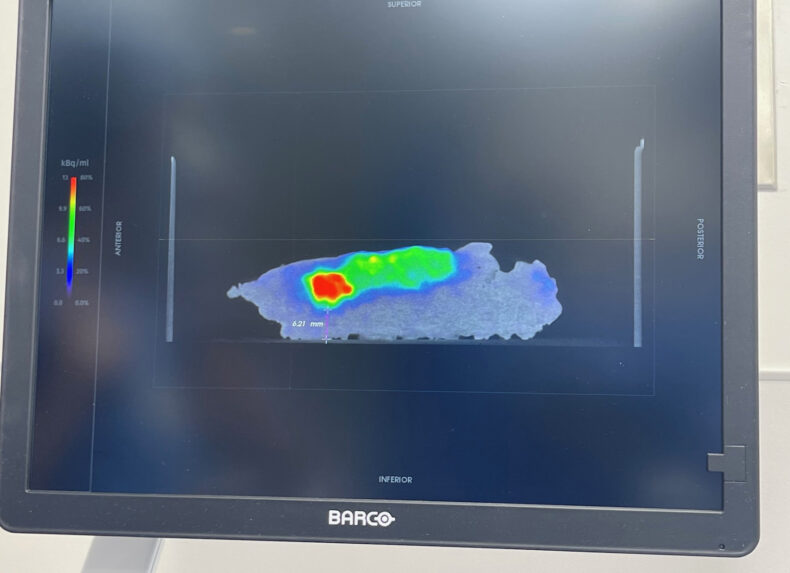
Topf explained that during surgery, a patient receives a dose of fluorodeoxyglucose (FDG), a radiopharmaceutical substance that helps light up the tumor in a PET scan. With the PET-CT scanning, as soon as the cancer is removed, it is placed in the scanner for margin analysis.
“We’re actively investigating both the feasibility of using this approach in the operating room during head and neck cancer surgery and whether it can accurately show cancer margins compared to the ‘gold standard’ of microscopic analysis,” said Topf.
Nicole Jones, research coordinator IV in the otolaryngology research laboratory, explained that that “gold standard” for cancer resection surgeries involves sending the specimen to the pathology lab for initial review. A full analysis of the resected tissue might not be available for several days. With the help of the intraoperative imaging device, however, critical information about the surgery’s success in achieving a negative margin could be available in a matter of minutes.
“The potential impact for patients and surgeons in real-time care is profound,” said Jones. “Instead of the surgeon having to leave the OR and go to the pathology lab, everything is done in real time. This is an incredibly exciting milestone, and we hope this innovation will lead to transformative results down the road and will eventually be widely used in clinical settings.”
Topf said the opportunity to participate in clinical research — and doing so without making more than one trip to the hospital — is an appealing way of contributing to science.
“For patients, it’s an exciting opportunity to participate in cutting-edge research and use a device that may allow a surgeon to have increased confidence in their ability to remove cancer, which is very attractive,” he said.
“This is a great new technology that will change our three-dimensional view of the tumor immediately after surgery, providing the surgeon critical information,” said Eben Rosenthal, MD, chair of the Department of Otolaryngology-Head and Neck Surgery.
Additionally, the procedure uses a lower dose of FDG, so on the day of the surgery, the patient is exposed to only 20% of radiation typically used for a whole-body PET-CT scan.
Marcus Balanky, director of Radiation Safety in the Office of Clinical and Research Safety (OCRS), said the new procedure demonstrates that radiopharmaceuticals can benefit multiple areas of a health care center’s clinical enterprise while protecting patient safety.
“This project is a great collaboration between Otolaryngology, Radiochemistry and OCRS Radiation Safety, highlighting the wide range of applications and effectiveness of radioactive material in research and clinical applications,” said Balanky.
Goals for the surgical team are to refine the workflow, demonstrate radiation safety in the operating room and show that the scanning process is as effective with the novel machinery in the OR space as it is when the sample is sent to the pathology lab for analysis, Topf said. He credited his team, specifically the research coordinators, for helping coordinate the PET-CT procedures that involve collaboration by many areas of the Medical Center.
“This was a very rewarding experience, and it has been amazing to see all the hard work our team put into this effort coming to fruition,” said Kyrionna Golliday, research coordinator II in the otolaryngology research laboratory.











