Vanderbilt-Ingram Cancer Center has treated its first patient in a newly launched therapy program that magnifies the power of a person’s natural defense system against tumors.
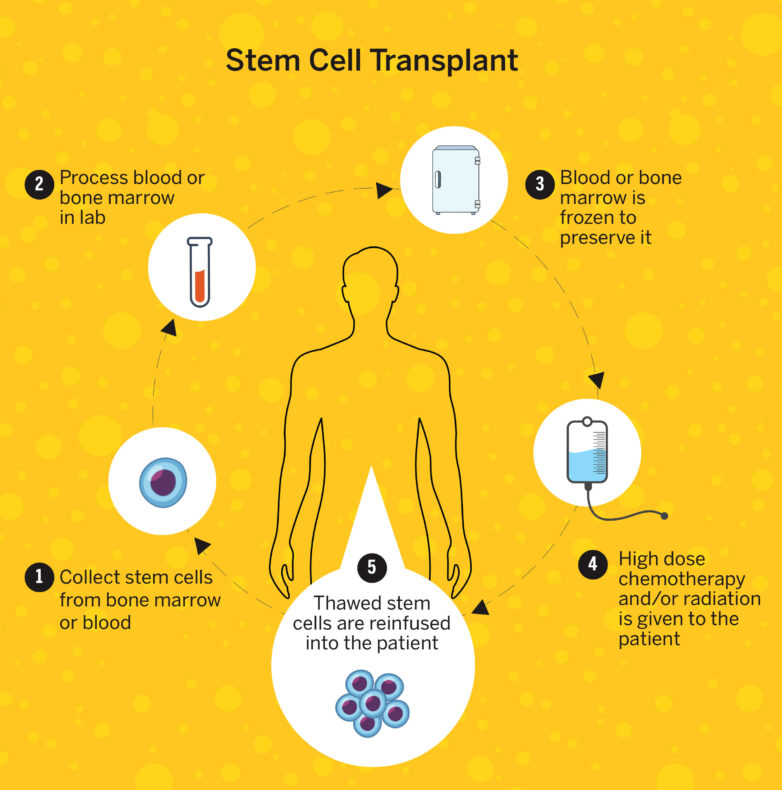
Tumor-infiltrating lymphocyte (TIL) therapy involves isolating the white blood cells from a tumor after it is surgically removed, expanding the magnitude of those cells in a laboratory, and then infusing them back into the patient to elicit a more powerful counterattack. The highly personalized treatment is currently approved for patients with advanced stages of melanoma whose tumors have grown despite immunotherapies and/or targeted therapies.
The patient who received the therapy in late January has melanoma that has spread to the bone, abdomen, liver and brain despite multiple lines of other treatments. A team of clinicians harvested white blood cells from a tumor in the patient’s liver, then shipped them to a laboratory where they were supercharged before being infused back into the patient, who is being monitored. Additional patients are scheduled to receive TIL therapy. Vanderbilt-Ingram launched the program as a standard of care service line after previously treating patients with TIL therapy in clinical trials.
“The mission of Vanderbilt Health is to get treatments that are cutting-edge to the patients who need them the most,” said Olalekan Oluwole, MBBS, MPH, associate professor of Medicine and a hematologist who specializes in cellular therapies. “Some of these patients have exhausted prior standard of care options.”
About a third of patients who receive TIL therapy respond to it.
“On the surface that doesn’t sound like a lot, but the great thing about TIL therapy is when it does work, it can lead to long-term durable response. It can keep right on working for years or even indefinitely,” said Douglas Johnson, MD, MSCI, professor of Medicine and clinical director of melanoma, who holds the Susan and Luke Simons Directorship.
Establishing the TIL program required assembling a team of multidisciplinary clinicians trained to handle the care needs of patients while simultaneously handling the logistics of getting their white blood cells shipped to a laboratory.
Sarah Moseley, BSN, RN, the coordinator for immune effector cell and gene therapy patient care, led that process. She described the process of navigating care for patients who receive TIL therapy, which involves surgeons, oncologists, hematologists and specialized nurses.
“I am with the patient from start to finish,” Moseley said. “Once a patient is identified by Dr. Johnson, he immediately gets me involved. The patient has to be approved by our cell therapy team and our surgery team as well as Dr. Johnson to make sure that they’re a good candidate. The next step is the insurance process, which is probably the hardest part because this is a new and expensive therapy. It is a detailed process involving our financial team, our managed care team and us nurses as well.”
The nurses serving as patient care coordinators also include Leslie Mader, BSN, RN, OCN, and Brittney Baer, BSN, RN.
“I or one of my nurse colleagues go to the surgery, and we transport the specimen from the operating room to the processing lab, where a courier picks it up,” Moseley said. “Without the specimen, there is no product for the therapy. It has to be done quickly, and it must be done right every time. Then we get the patients set up for cell infusion after about five to six weeks.”
The launch of the TIL program is the latest achievement in cellular therapies for Vanderbilt-Ingram, which is an international leader in the field. The cancer center offered clinical trials for therapies, which became standards of care, most notably CAR-T, which is shorthand for chimeric antigen receptor T-cell therapy. Vanderbilt-Ingram established an outpatient protocol for patients to receive CAR-T and treats more patients with this immunotherapy than any other provider in the state. It is offering clinical trials to expand the treatment for additional types of cancer and to make it more easily accessible to patients.
“The launch of our TIL program represents a natural and important evolution of Vanderbilt-Ingram’s leadership in cellular therapy,” said Ben Ho Park, MD, PhD, the Benjamin F. Byrd Jr. Professor of Oncology, professor of Medicine and director of Vanderbilt-Ingram Cancer Center. “Building on the infrastructure, clinical expertise and multidisciplinary coordination established through our CAR-T program, we are now able to offer another highly personalized immunotherapy to patients with otherwise limited options. Our goal is not only to deliver these complex therapies safely and effectively, but also to continue advancing the science so that more patients, across more cancer types, can benefit in the years ahead.”
Clinicians with the cellular therapy team built the TIL program on the foundation of the CAR-T program. However, there are major differences between these treatment modalities. With CAR-T, immune cells are reengineered to attack cancer from the T cells in a patient’s blood. With TIL therapy, white blood cells are taken from a patient’s tumor and are then multiplied so they can stage a better counterattack against cancer.
Currently, CAR-T is approved by the Food and Drug Administration only for certain blood cancers. TIL therapy is approved only for advanced melanoma when patients have not responded to other treatments. However, clinical trials are underway to expand the therapies for other types of cancers.