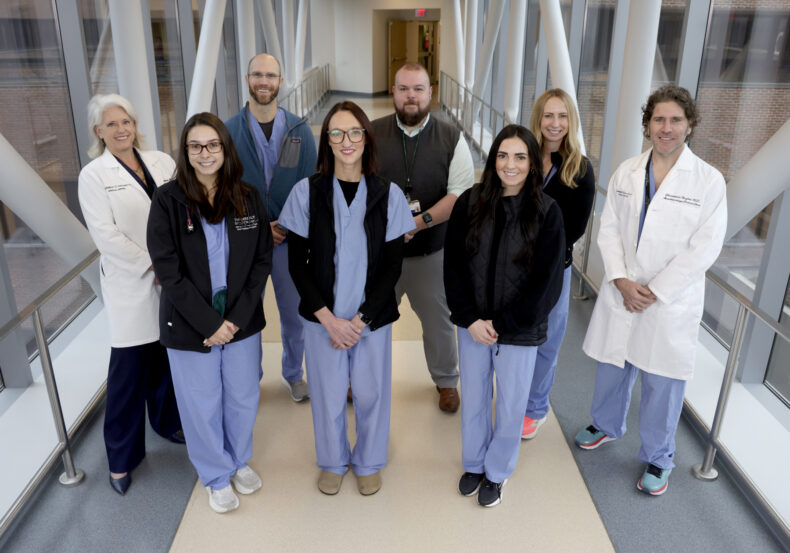
 Some members of the Critical Care Outreach Team at Vanderbilt University Hospital include, front row, left to right, Casey Ernfelt, ACNP, Lindsay Trantum, ACNP, Rebekah Pike, ACNP. Back row, left to right, Liza Weavind, MBBCh, Cody Bowers, AG-ACNP, Kipp Shipley, DNP, Megan Shifrin, DNP, ACNP-BC, and Christopher Hughes, MD. (photo by Donn Jones)
Some members of the Critical Care Outreach Team at Vanderbilt University Hospital include, front row, left to right, Casey Ernfelt, ACNP, Lindsay Trantum, ACNP, Rebekah Pike, ACNP. Back row, left to right, Liza Weavind, MBBCh, Cody Bowers, AG-ACNP, Kipp Shipley, DNP, Megan Shifrin, DNP, ACNP-BC, and Christopher Hughes, MD. (photo by Donn Jones)
If you spot a group of individuals in medical scrubs carrying bright orange sling backpacks moving briskly through Vanderbilt University Hospital (VUH), know that help is on its way.
They’re members of the Critical Care Outreach Team (CCOT) on a rapid response call, rushing to provide immediate medical assistance to a patient in a non-intensive care unit bed. Their job is to quickly assess and work to stabilize the patient, with the goal of averting a more serious medical crisis or death.
Since January 2020, members of the VUH CCOT have responded to more than 10,000 rapid response calls in every non-ICU unit in the adult hospital. It takes five minutes or less for the team to be at a patient’s bedside delivering interventions to prevent further health deterioration.
“Our rapid response system and our Critical Care Outreach Team have truly transformed the safety culture at VUH and made some remarkable interventions,” said Liza Weavind, MBBCh, MMHC, VUH associate chief of staff and professor of Anesthesiology and Surgery. “Despite the increasing acuity of our patients and increasing capacity at VUH, through the addition of this service, we have maintained an ICU transfer rate of around 30% without an increase in out-of-ICU cardiorespiratory arrests or the need for second or third RRT responses for the same patient.”
The CCOT is made up of advanced practice providers (APPs), including nurse practitioners and physician assistants, and a virtual intensivist (physician specializing in critical care medicine). Team members are strategically based in the hospital so they can respond to any patient unit rapidly.
While the team responds to the patient’s room, the virtual intensivist is already reviewing the patient’s electronic health record (EHR) for their history, recent labs, imaging, vital sign trends and other critical information to guide the action plan. By January 2026, virtual nursing cameras installed in non-ICU rooms will allow the intensivist to join a rapid response more seamlessly, Weavind said.
The team’s goal is to intervene when early warning signs of clinical deterioration are recognized. Those signs include vital sign changes; labored breathing; chest pain; uncontrolled bleeding from a surgical site or port; decreased consciousness; increased agitation or delirium; seizure; and other changes in mental status. The majority of rapid responses since 2020 have been due to cardiovascular (41%) and respiratory issues (22%), followed by neurological issues (19%), general concern (3%) and uncontrolled bleeding (2%).
Bedside interventions can include labs and blood draws, stabilization of airway/breathing and administration of medication. The rapid response team also determines whether a patient should be transferred or “escalated” to an ICU for elevated care. Patients can also be referred to palliative care, hospice or another care arrangement that best fits the individual’s medical needs and goals of care.
They work in collaboration with the patient’s primary care team on the unit, as well as with family members. If the decision is made to escalate a patient to ICU care, they are transported safely to a “just-in-time” ICU bed designated for this purpose, Weavind said.
This team differs from the hospital’s STAT team which responds to cardiorespiratory arrests and near arrests experienced by patients, visitors and staff on VUH grounds, though a CCOT NP also responds with the STAT team to document the actions taken so the team can focus on saving lives.
At VUH, staff, visitors and patients can call the emergency number, 1-1111, to activate an emergency response team. Emergency medical dispatchers with LifeFlight Communications answer the call, quickly evaluate the situation and dispatch the appropriate responders.
Today, the CCOT includes 15 full-time NPs, who no longer wear orange but carry bright orange gear bags, and 15 intensivists. There are two APPs and an intensivist ready to respond on every shift around the clock. In 2024, the team was enhanced by combining CCOT with the Critical Care APP Float Pool.
The combined model follows a block schedule, with eight weeks working in ICUs and eight weeks running rapid response calls with the CCOT. The NPs rotate through the ICUs, which include the medical, surgical, neurological, cardiovascular, trauma and burn units, so they gain specialized knowledge in each area to better manage a wide range of patient populations.
“When we send our float pool NPs to an ICU, there’s an obvious benefit to the ICU in terms of improved staff coverage, less overtime and reduced burnout, but we’re also cross-training our team so they continue to grow as clinicians,” said APP Float Pool Lead Cody Bowers, MSN. “And when our NPs work in the different ICUs and then with the CCOT on rapid responses, they gain a great deal of institutional, logistical knowledge.”
Beyond the obvious need for critical care skills, the NPs must be able to communicate clearly and effectively with a variety of medical providers, patients and their families, said CCOT Lead Kipp Shipley, DNP.
“We interface with every single team in the hospital — even teams that aren’t in the hospital, such as our ambulatory teams,” Shipley said. “Inherent in our work is the ability to find common ground and work toward the best outcomes for our patients and our staff, and to be able to navigate difficult conversations. When we onboard employees to the CCOT, one of the first things we tell them is that this is 70% communication and 30% clinical work.”
“The team has really become the go-to resource for the hospital for any kind of emergency deterioration outside the norm.” Weavind said. “We have the most incredible team members who understand the system, who are able to give our patients a timely, consistent response and support our nursing staff on the floors. I really can’t take my hat off to this team enough.”











